You’ve taken an oath as a healthcare provider to provide the best possible care to your patients. However, as the owner of a practice, you must also take care of the financial side of your business. It is critical that you or your staff follow the 10 steps in the medical billing process as part of your revenue cycle management.
This process begins when a patient comes to you, either in person or remotely (via telemedicine, for example), and ends when you receive payment. There will be communication between you and your patient, as well as between you and your staff, as well as between your office and health insurers.
It can appear complicated at times, especially if you’re just starting out in private practice. However, if you consistently follow the medical billing process, you will streamline the process, reduce errors, and receive payment for your services on time.
10 Steps in the Medical Billing Process
These ten steps in the medical billing process will provide a strong foundation for the business side of your practice. The healthcare industry (hospitals, insurance companies, private practices, and patients) loses billions of dollars annually due to billing errors. This procedure will aid in minimizing those errors.
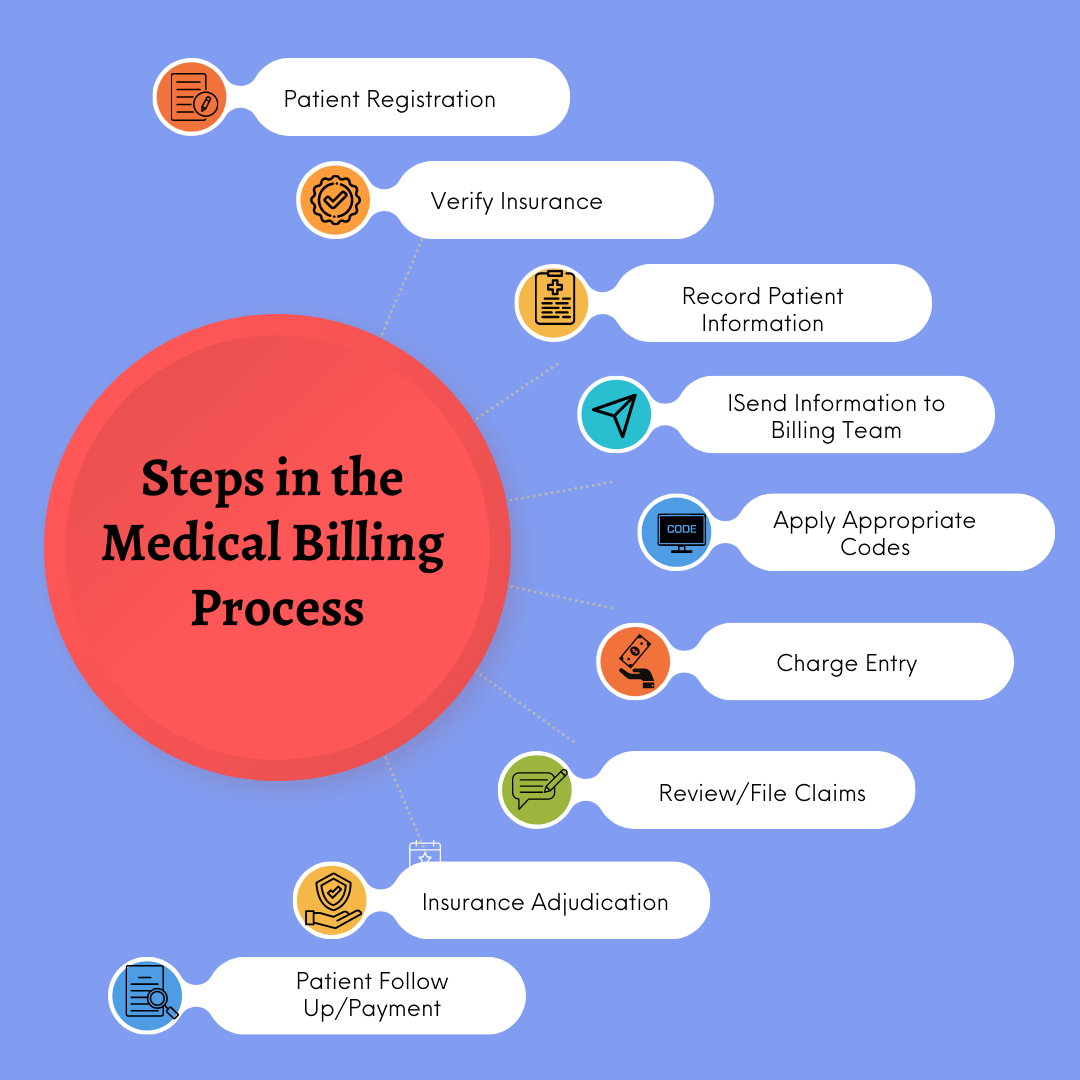
Patient Registration
Every visit, whether a patient is seeing you for the first time or has been seeing you for a decade, must include some form of patient registration. For a first-time visit, a complete medical history, including demographic information, should be obtained for record-keeping purposes.
Even if the patient is a regular, double-check key details (address, phone number, insurance, etc.) to ensure the file is completely up to date. Confirming an address or date of birth right away ensures that new information is added to the correct patient’s file.
Verify Insurance, Financial Responsibility
Ensure that you have current and accurate insurance coverage on file for the patient during patient registration. Depending on the nature of the visit (worker’s compensation, accident, etc.), you’ll want to know if any additional charges must be billed.
This step allows you to ensure that you have the correct insurance information, that the patient is currently covered, and that you have reviewed their out-of-pocket expenses. Confirming this information will help to avoid future delays and billing errors.
Record Patient Information During Visit
Take down all of the information shared during the appointment during the visit. If possible, record the meeting (audio or video) or take meticulous notes—all of this information will need to be given to a medical coder after the visit so that the appropriate codes can be applied.
Following the visit, the meeting can be transcribed. Check that the reason for the visit is clear, that any diagnoses are included, that any prescriptions are listed, and so on. Not only will this benefit your coding/billing team, but it will also provide your patient with a more comprehensive medical history for future use.
Send Patient Information to Billing Team
This medical transcription, also referred to as a medical script, is then cleaned up and prepared for the medical billing team. If this is done internally, you can send the audio recording to your staff so that they can transcribe the notes. If a third party is handling your billing, ensure that the medical script is error-free.
This is a crucial phase of the process where many errors can occur. If you are clear, concise, and thorough during the transcription process, you will make the lives of your coders, medical billers, and patients much easier.
Apply Appropriate CPT Codes
You or your staff of coders will assign the correct CPT or HCPCS code to the services you performed. Carefully select the code that most precisely reflects the service rendered, and confirm that the component services are not billed separately if they are bundled with the primary procedure.
Next, you or your coders must select the correct ICD-10 diagnosis codes for the patient. There are approximately 68,000 unique codes to choose from. The previous version (ICD-9) had approximately 13,000 codes to choose from; ICD-10 has nearly five times as many. This is one reason why the information you record in the patient’s medical record is so crucial.
Charge Entry
Based on the codes assigned to the visit, your billing team will now prepare a medical claim. That is why it is critical to use the correct codes—an incorrect code can drastically alter the charges. And, while the codes are uniform, the fees are not.
Ensure that all fees are listed, as well as the appropriate visit codes. By clearly itemizing medical services, you can reduce errors and streamline the process. Any errors here could result in claim denials and non-payment or reimbursement from the insurer. It can also have an impact on how much your patient has to pay out of pocket.
Review, File Claims
The claims are submitted for reimbursement after they have been reviewed for accuracy. This can be done electronically and usually involves a scrubbing phase followed by another review process. Software ensures that all form fields are completed and that the corresponding codes and fees are correct.
The claims are then routed to a clearing house for final review. They perform a final check of basic information (name, active insurance checks, date of birth, and so on) before reformatting the claim for specific payers—not all payers use a standard format.
Insurance Adjudication/Reimbursement Process
This is when the insurance company will review the claim for covered services or procedures and accept or deny it. If there are errors, the claim will be denied, along with a detailed explanation and steps to correct any problems. The claim can then be resubmitted.
In some instances, the claim may be denied because the insurer does not cover the services. This is where the work done at the beginning of the process pays off, particularly in terms of the patient’s insurance coverage. Now is a terrible time to discover that they do not have coverage when they previously believed they did.
Prepare Patient Statement
Assuming everything is accurate, a statement for your patient is prepared. If there is a non-zero balance, the charges and benefits received from the insurer should be clearly explained. This will explain why there are fees and how much they are. Include payment instructions, due dates, and even ways for a patient to file an insurance claim.
Patient Follow Up/Payment
The final step in the process is receiving payment from the insurer and the patient. When claims are accepted by insurance companies, payments are frequently made automatically. Patients can pay for a visit in advance (co-pay) or before the procedure. Others may choose to pay at various times.
Although each step is critical, getting paid for your services is what allows you to make money, pay your employees, and keep the lights on. You must give your patients a certain amount of time to begin paying, but you may be forced to go through collections.

